Kirstin promised I'd send some pseudo-medical details, so here they are. Remember I'm enthusiastic about this stuff, but not necessarily accurate so all of you orthopaedic surgeons out there, cool it!
Dr Alkheryf is planning only on addressing C1-C2 fusion at this point, and if nothing goes wrong during the surgery, that's what he'll stick to. Three (or four) options:
- Wire between C1/C2 with a bone graft. Okay, not super strong, but fairly easy to do.
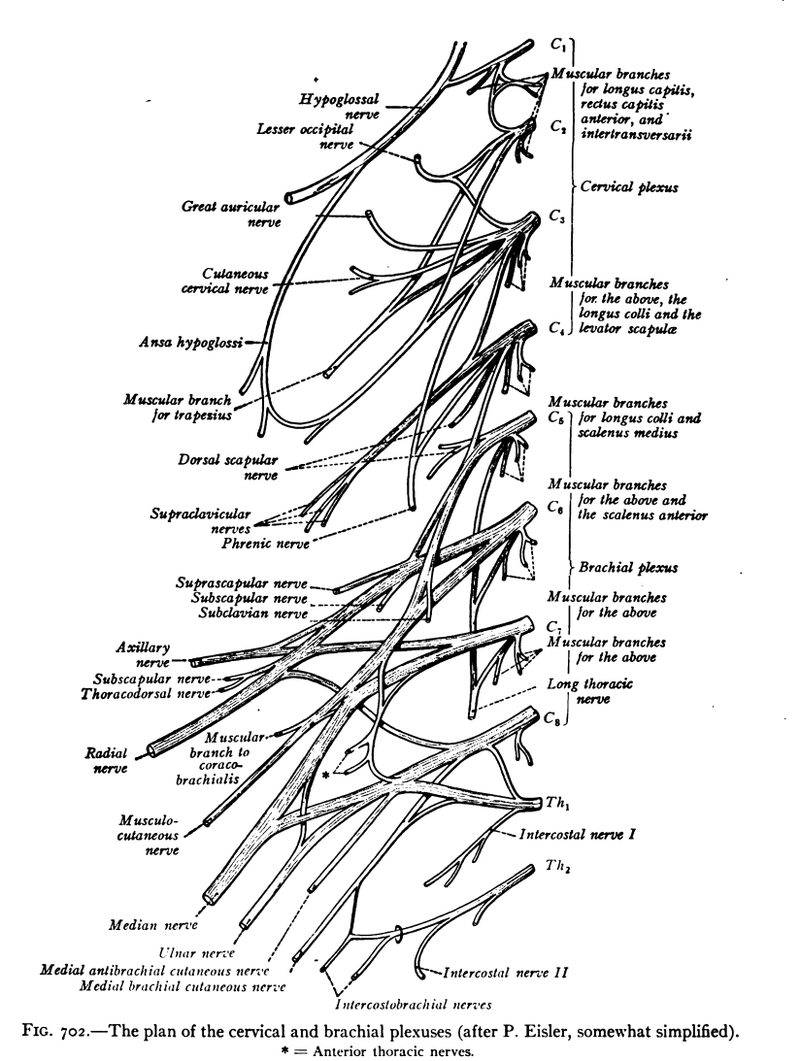
- Screws and rods. As seen in my animation video I'd linked to previously - four screws in total (left pair, right pair) then a rod that connects each pair vertically). Dr A's preferred technique. Includes bone graft. Requires lifting the nerves which is a little risky (though I didn't ask which ones - see the schematic above.
- A single longer screw that goes from C2 up to C1 (on each side, two screws in total). Easier to avoid the nerves, slightly riskier for hitting a vertebral artery).
- The option he doesn't want to fall back on, but if absolutely necessary - adding a plate to the occiput and doing an occipital-C1-C2 fusion. Less risk of artery damage, but massive limitation to motion. This might happen if the bones are really not robust enough to anchor the screws - something that can be estimated by the CT scan (and they look okay at the moment) but won't really be know until they are drilling the holes.
The bone graft choices are to take some from the hip (another incision, potential infection site, own-bone-is-best, might not be great bone, no negative effects on hips) or to use some artificial bone (not as good as home-grown, no other incision needed). Dr A. plans on using some of both (though I'm not 100% sure why this is a better option than just pure Kirstin...?).
The non-surgical options at this point are limited to a life-long neck brace (which will become a vicious circle as her neck muscles atrophy through lack of use, increasing the instability).
In terms of motion restriction afterwards, we should expect about 30-50% reduction in flexion (nodding) but very little in rotation. Kirstin will say no more easily than yes... Recovery should take 3-6 months and will not require a halo (phew - she can be insufferable as it is when she's right!) which, in case you haven't seen one, gets screwed into the skull. That's a relief all round. And no stay in rehab should be necessary, just some out-patient physio therapy.
Dr A was great about offering to make a referral if we wanted one, either for a second opinion or just to have someone else operate.
So, that about covers it! Kirstin signed on the dotted line immediately, having thought most of this stuff through before thanks especially to Dr Johnson in Australia (why would you not trust a Johnson?) who had given us a great primer and
